Strategies to prevent an individual’s fracture risk
backed by guidelines on post-fracture care
1. Assess for osteoporosis and fracture risk1
- Women and men over age 50 should be assessed for risk factors
- Measure height annually
- Assess for the presence of vertebral fractures
- Assess history of falls in the past year
- If a fall did occur, a multifactorial risk assessment (i.e., the ability to get out of a chair without using arms) should be conducted
2. Order guideline-recommended biochemical investigations as needed for patients with osteoporosis1
3. Assess for 10-year risk of a major osteoporotic fracture1
Evaluate your patient’s risk of a fracture of the hip, vertebra, forearm or proximal humerus using one of the following tools:
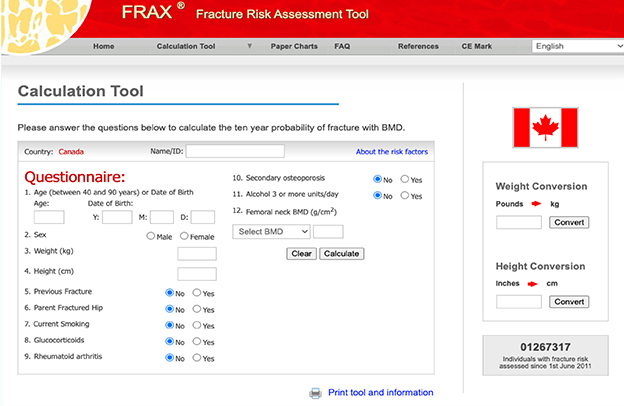
The WHO Fracture Risk Assessment tool is based upon a more complete set of clinical risk factors and can be used even without results for bone mineral density, but the calculations require access to the system’s software, website or paper charts. The 2010 version of the Canadian Association of Radiologists and Osteoporosis Canada tool is less complete but is easier to use.
– 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada (summary)1
4. Promote patient-led bone health strategies2
- Balanced nutrition2
- Adequate calcium and vitamin D intake2
- Physical activity: resistance training and weight-bearing exercises2
- Avoid smoking and excessive alcohol intake2
5. Apply an integrated treatment approach to manage patients at risk of a fracture1
The guidelines recommend an integrated approach that will consider the patient’s individual risk profile, comorbid conditions, preferences and lifestyle. This approach may include:
- Initial BMD testing
- Assessment of fracture risk
- Exercise and prevention of falls (exercise that enhances core stability, focuses on balance and use of hip protectors)
- Calcium and vitamin D intake recommendations
- Other recommendations from the 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada
6. Create a Bone Health Care Plan
Consider the Bone Health Patient Journey to help identify where to support your patient and which clinic partner can best support them.
Bone health is a team sport
Work with your Clinic Partners to ensure important steps are taken to prevent and manage fracture risk.
CLINIC PARTNER ROLES

- When checking in the patient, ask if they have fractured or fallen recently
- Conduct an EMR Query to ID patients who haven’t been seen in person since COVID or who have not filled their Bone Health prescription
- Complete patient support program associated administrative needs
- Schedule and conduct bone health patient check-in calls

- Ask questions to help ID patients at risk of fracture, for example:
- Have you fractured or fallen recently?
- Assess smoking, alcohol intake & other risk factors as per CPG*
- Conduct accurate weight & height measurement: flag if >2 cm height loss
- Counsel and support
- Enrol in patient support program or create reminder system to support patient compliance

- Offer consistent and accessible support for patient and caregivers
- Provide information, education and answering questions
- Liaise with the patient’s circle of care of healthcare professionals
- Conduct medication reviews and Opinion Letters for at-risk patients
* CPG = Canadian Practice Guidelines; EMR= electronic medical record




