Understanding the osteoporosis care gap in Canada
Insights from the Public Health Agency of Canada (PHAC) Osteoporosis and Related Fractures in Canada report1
Based on administrative health data from the Canadian Chronic Disease Surveillance System 2015-2016 with trend data spanning the 15-year period 2000-2001 to 2015-2016.

Osteoporosis care gap
Despite well-established clinical practice guidelines and initiatives to promote osteoporosis care, rates of patient screening and initiation of Bone Health Care Plans following a fracture remain very low.1
Osteoporosis Canada’s 2010 clinical practice guidelines call for bone mineral density (BMD) testing in anyone who has had a fragility fracture after age 40, as well as in both women and men aged 65 years and older.1
The recommended management model is based on the assessment of fracture risk, which is in part based on BMD.1,2

However, within the year following an osteoporosis‑related fragility fracture, data have shown:1
- Less than 10% of Canadians aged 40+ had a BMD test1
- Men were less likely than women to receive a BMD test following a fracture

Multiple factors contribute to the osteoporosis care gap1
Lack of:
- Awareness of the increased risk of refracture
- Integration between hospital and community health services
- Recognition of the burden of fragility fracture
- Prioritization in terms of management
- Investment in dedicated coordinated strategies for secondary fracture prevention
The osteoporosis care gap can have life-changing consequences. Watch these videos to learn more.
Narrowing the osteoporosis care gap: focus on absolute fracture risk

Can the gap be narrowed?
PHAC report: Shift the focus of osteoporosis care from low BMD to preventing fractures
Canadian guidelines: Focus on absolute fracture risk to decide on next steps in the individual’s care, incorporating clinical risk factors beyond low BMD1,2
Shift the focus of osteoporosis care from low BMD to preventing fractures
To make the shift, the PHAC report recommends that healthcare practitioners focus on an individual’s fracture risk to decide on next steps in their care with a:
fracture risk assessment1,2 and

a Bone Health Care Plan based on high absolute fracture risk, which incorporates clinical risk factors beyond low BMD.1,2

Case finding and fracture risk pyramid using an approach that targets an entire population for fracture risk assessment.2

Based on Figure 16 in PHAC 20201
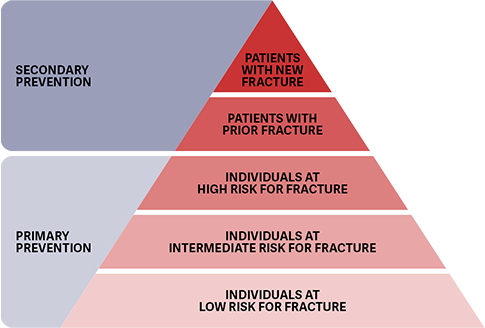
To determine an individual’s fracture risk, the case finding and fracture risk approach (promoted in the PHAC report and supported by the 2010 Canadian Guidelines) recommends dividing the entire population into those who have a fracture history (secondary prevention) and those who have yet to have a fracture (primary prevention).1-3
This case finding approach ensures those with new fractures get immediate attention, while those patients with osteoporotic fragility fractures also receive the care they need.2
Based on Figure 16 in PHAC 20201






